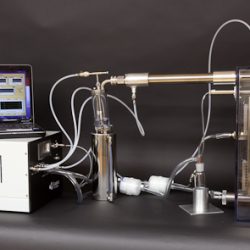
Biaera’s whole body Inhalation system for infectious agents integrates the Aero3G control platform with a whole body exposure chamber. The 38 Liter chamber was originally developed for aerosol exposures of mice [Stephenson (1988)], and has been used for exposures with a variety of infectious agents in a variety of conditions.
[Jeddeloh (2003); Roy (2003); Heine (2007); Roy (2009); Gustin (2011)].
General Description
The whole body chamber operates in a “push-pull” modality, meaning that aerosol is constantly being supplied to and exhausted from the chamber. This dynamic exposure method ensures that the infectivity of the infectious agent is not compromised by an extended residence time in the chamber. This chamber operates at a recommended flow rate of 19 LPM, resulting in an aerosol residence time of two minutes. All of the flow rates to and from the chamber are managed by the Aero3G control platform. Test subjects or other materials are held in perforated cages during the aerosol exposure. Perforated cages are available in a variety of shapes and sizes. Plants, equipment and other materials can also be placed in the chamber without cages.
The chamber is outfitted with probes to monitor the chamber pressure, relative humidity, and temperature through the Aero3G control system. The Aero3G uses the pressure measurement to ensure that the ambient pressure condition in the chamber does not increase or decrease and pose a hazard to test subjects or other exposed materials. The humidity measurement combines with the Aero3G humidification system to maintain a stable, user-defined relative humidity. Deviations in relative humidity can adversely affect the infectivity of agents in aerosols. This control feedback ensures consistency within and across studies for a given agent.
The temperature measurement combines with a user-defined temperature range in the AeroMP software to provide assurance that test subjects or other materials are not experiencing unsuitable conditions during the exposure process.
Aerosols are generated with a three-jet collision nebulizer. The collision has been a primary aerosol generation device in the infectious aerosol research community [Stephenson (1988); Jeddeloh (2003); Roy (2003); Hartings and Roy (2004); Heine (2007); Roy (2009), Nalca (2010); Gustin (2011)]. It combines ease-of-use, durability, and reliability in high containment aerosols with a consistent record of producing bioaerosols without adversely affecting the infectivity of biologics. Control, monitoring, and recording of the collison operation are all managed through the Aero3G control platform.
Aerosol sampling is accomplished with a 6 LPM all-glass impinger. The all-glass impinger also has an established history in infectious disease research with a variety of agents [Stephenson (1988); Jeddeloh (2003); Roy (2003); Hartings and Roy (2004); Heine (2007); Roy (2009), Nalca (2010)]. The impinger collects a sample of the aerosol during the exposure. Subsequent analysis and enumeration of the sample provides confirmation of aerosol characteristics and provides the basis for calculating the inhaled dose to test subjects or exposure concentration to other materials. While impingers of various flow rates are available, the 6 LPM impinger is sufficient to achieve a high sampling efficiency while not disrupting the flow dynamics in the whole body chamber. Control, monitoring, and recording of the impinger functions are all achieved through the Aero3G control platform.
This particular implementation of the Aero3G is just one illustration of the capabilities of this technology. Similar configurations can be assembled with virtually any existing chamber, aerosol generator, monitor, or sampling device. Contact Biaera Technologies to discuss options for your laboratory.
References
- KM Gustin, JA Belser, DA Wadford, MB Pearce, JM Katz, TM Tumpey, and TR Maines. (2011). Influenza virus aerosol exposure and analytical system for ferrets. Proceedings of the National Academy of Science 108(20):8432 doi: 10.1073/pnas. l 100768108.
- JM Hartings and CJ Roy. (2004). The automated bioaerosol exposure system: platform development and a dosimetry application with nonhuman primates. Journal of Pharmacological and Toxicological Methods 49:39.
- HS Heine, J Bassett, L Miller, JM Hartings, BE Ivins, MLM Pitt, D Fritz, SL Norris, and RW Byrne. (2007). Determination of antibiotic efficacy against Bacillus anthracis in a mouse aerosol challenge model. Antimicrobial Agents and Chemotherapy 51:1373.
- JA Jeddeloh, DL Fritz, DM Waag, JM Hartings, and GP Andrews. (2003). A bio-defense driven murine model of pneumonic melioidosis. Infection and Immunity 71:584.
- A Nalca, VA Livingston, NL Garza, EE Zumbrun, OM Frick, JL Chapman, and JM Hartings. (2010). Experimental infection of Cynomologus Macaques (Macaca fascicularis) with aerosolized Monkeypox Virus. PLoS One 5:e12880.
- CJ Roy, M Hale, JM Hartings, MLM Pitt, and S Duniho. (2003). Impact of inhalation exposure modality and particle size on the respiratory deposition of ricin in BALB/c mice. Inhalation Toxicology 15:619.
- CJ Roy, DS Reed, CW Wilhelmsen, JM Hartings, S Norris, and KS Steele. (2009). Pathogenesis of aerosolized Eastern Equine Encephalitis infection in guinea pigs. Virology 6:170.
- EJ Stephenson, RB Moeller, CG York, and HW Young. (1988). Nose-only versus whole-body aerosol exposure for induction of upper respiratory infectious oflaboratory mice. American Industrial Hygiene Association Journal 49:128.